The market for true wireless stereo (TWS) active noise canceling (ANC) hearables (headphones and earbuds) has been soaring in recent years, and the global shipment volume will nearly double that of smart wristbands and watches in 2023. The on-head time for hearables has extended significantly due to the recent advances in ANC, transparency mode, and artificial intelligence. Users frequently wear hearables not just for music listening, but also for exercising, focusing, or simply mood adjustment. However, hearable health is still mostly uncharted territory for the consumer market.
In “APG: Audioplethysmography for Cardiac Monitoring in Hearables,” presented at MobiCom 2023, we introduce a novel active in-ear health sensing modality. Audioplethysmography (APG) enables ANC hearables to monitor a user's physiological signals, such as heart rate and heart rate variability, without adding extra sensors or compromising battery life. APG exhibits high resilience to motion artifacts, adheres to safety regulations with an 80 dB margin below the limit, remains unaffected by seal conditions, and is inclusive of all skin tones.
 |
| APG sends a low intensity ultrasound transmitting wave (TX wave) using an ANC headphone's speakers and collects the receiving wave (RX wave) via the on-board feedback microphones. The APG signal is a pulse-like waveform that synchronizes with heartbeat and reveals rich cardiac information, such as dicrotic notches. |
Health sensing in the ear canal
The auditory canal receives its blood supply from the arteria auricularis profunda, also known as the deep ear artery. This artery forms an intricate network of smaller vessels that extensively permeate the auditory canal. Slight variations in blood vessel shape caused by the heartbeat (and blood pressure) can lead to subtle changes in the volume and pressure of the ear canals, making the ear canal an ideal location for health sensing.
Recent research has explored using hearables for health sensing by packaging together a plethora of sensors — e.g., photoplethysmograms (PPG) and electrocardiograms (ECG) — with a microcontroller to enable health applications, such as sleep monitoring, heart rate and blood pressure tracking. However, this sensor mounting paradigm inevitably adds cost, weight, power consumption, acoustic design complexity, and form factor challenges to hearables, constituting a strong barrier to its wide adoption.
Existing ANC hearables deploy feedback and feedforward microphones to navigate the ANC function. These microphones create new opportunities for various sensing applications as they can detect or record many bio-signals inside and outside the ear canal. For example, feedback microphones can be used to listen to heartbeats and feedforward microphones can hear respirations. Academic research on this passive sensing paradigm has prompted many mobile applications, including heart rate monitoring, ear disease diagnosis, respiration monitoring, and body activity recognition. However, microphones in consumer-grade ANC headphones come with built-in high-pass filters to prevent saturation from body motions or strong wind noise. The signal quality of passive listening in the ear canal also heavily relies on the earbud seal conditions. As such, it is challenging to embed health features that rely on the passive listening of low frequency signals (≤ 50 Hz) on commercial ANC headphones.
Measuring tiny physiological signals
APG bypasses the aforementioned ANC headphone hardware constraints by sending a low intensity ultrasound probing signal through an ANC headphone's speakers. This signal triggers echoes, which are received via on-board feedback microphones. We observe that the tiny ear canal skin displacement and heartbeat vibrations modulate these ultrasound echoes.
We build a cylindrical resonance model to understand APG’s underlying physics. This phenomenon happens at an extremely small scale, which makes the raw pulse signal invisible in the raw received ultrasound. We adopt coherent detection to retrieve this micro physiological modulation under the noise floor (we term this retrieved signal as mixed-down signal, see the paper for more details). The final APG waveform looks strikingly similar to a PPG waveform, but provides an improved view of cardiac activities with more pronounced dicrotic notches (i.e., pressure waveforms that provide rich insights about the central artery system, such as blood pressure).
 |
| A cylindrical model with cardiac activities ℎ(𝑡) that modulates both the phase and amplitude of the mixed-down signal. Based on the simulation from our analytical model, the amplitude 𝑅(𝑡) and phase Φ(𝑡) of the mixed-down APG signals both reflect the cardiac activities ℎ(𝑡). |
APG sensing in practice
During our initial experiments, we observed that APG works robustly with bad earbuds seals and with music playing. However, we noticed the APG signal can sometimes be very noisy and could be heavily disturbed by body motion. At that point, we determined that in order to make APG useful, we had to make it more robust to compete with more than 80 years of PPG development.
While PPGs are widely used and highly advanced, they do have some limitations. For example, PPGs sensors typically use two to four diodes to send and receive light frequencies for sensing. However, due to the ultra high-frequency nature (hundreds of Terahertz) of the light, it's difficult for a single diode to send multiple colors with different frequencies. On the other hand, we can easily design a low-cost and low-power system that generates and receives more than ten audio tones (frequencies). We leverage channel diversity, a physical phenomenon that describes how wireless signals (e.g., light and audio) at different frequencies have different characters (e.g., different attenuation and reflection coefficients) when the signal propagates in a medium, to enable a higher quality APG signal and motion resilience.
Next, we experimentally demonstrate the effectiveness of using multiple frequencies in the APG signaling. We transmit three probing signals concurrently with their frequencies spanning evenly from 30 KHz to 32 KHz. A participant was asked to shake their head four times during the experiment to introduce interference. The figure below shows that different frequencies can be transmitted simultaneously to gather various information with coherent detection, a unique advantage to APG.
The 30 kHz phase shows the four head movements and the magnitude (amplitude) of 31 kHz shows the pulse wave signal. This observation shows that some ultrasound frequencies might be sensitive to cardiac activities while others might be sensitive to motion. Therefore, we can use the multi-tone APG as a calibration signal to find the best frequency that measures heart rate, and use only the best frequency to get high-quality pulse waveform.
After choosing the best frequency to measure heart rate, the APG pulse waveform becomes more visible with pronounced dicrotic notches , and enables accurate heart rate variability measurement.
 |
| The final APG signal used in the measurement phase (left) and chest ECG signal (right). |
Multi-tone translates to multiple simultaneous observations, which enable the development of array signal processing techniques. We demonstrate the spectrogram of a running session APG experiment before and after applying blind source separation (see the paper for more details). We also show the ground truth heart rate measurement in the same running experiment using a Polar ECG chest strap. In the raw APG, we see the running cadence (around 3.3 Hz) as well as two dim lines (around 2 Hz and 4 Hz) that indicate the user’s heart rate frequency and its harmonics. The heart rate frequencies are significantly enhanced in signal to noise ratio (SNR) after the blind source separation, which align with the ground truth heart rate frequencies. We also show the calculated heart rate and running cadence from APG and ECG. We can see that APG tracks the growth of heart rate during the running session accurately.
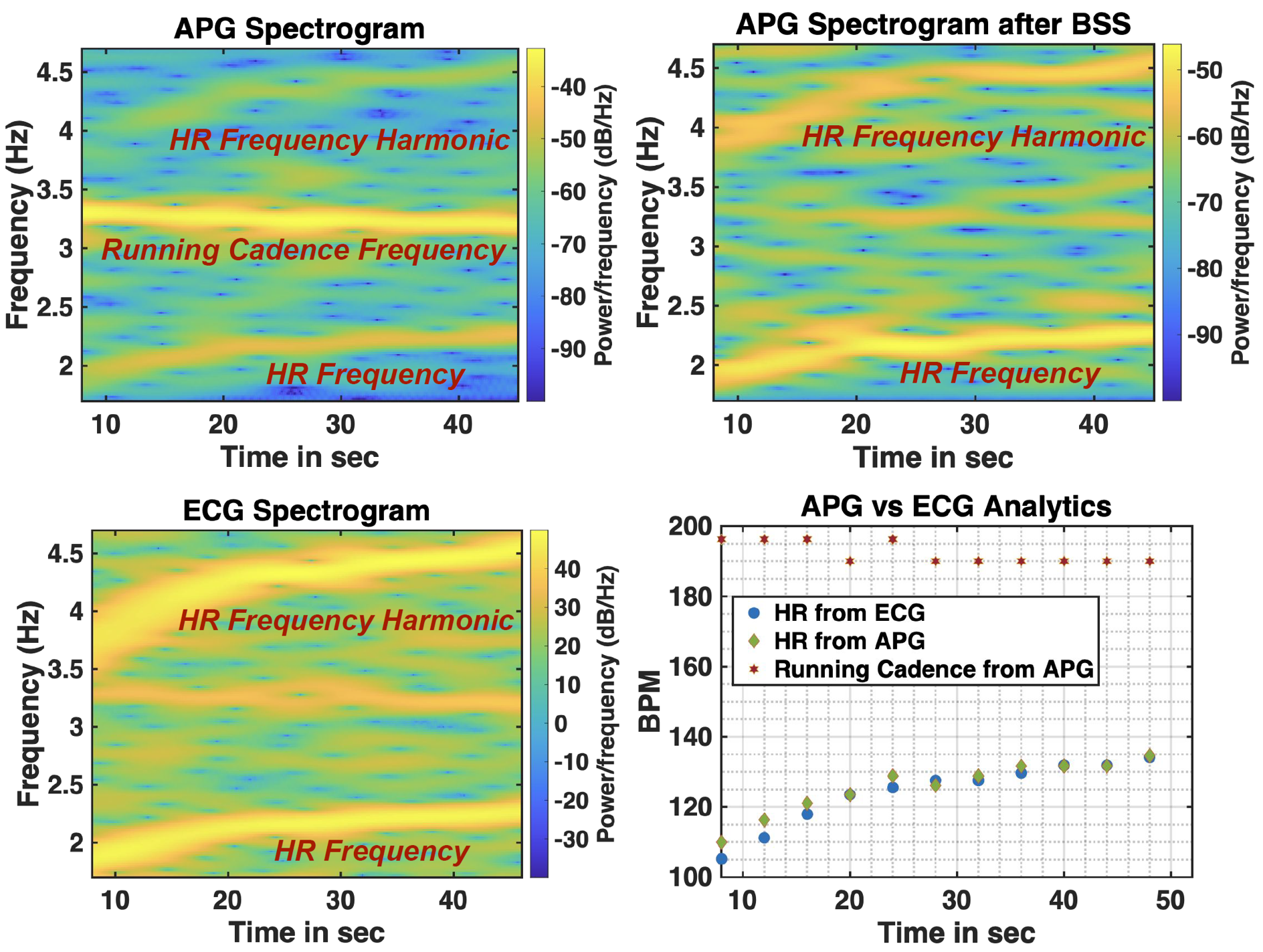 |
| APG tracks the heart rate accurately during the running session and also measures the running cadence. |
Field study and closing thoughts
We conducted two rounds of user experience (UX) studies with 153 participants. Our results demonstrate that APG achieves consistently accurate heart rate (3.21% median error across participants in all activity scenarios) and heart rate variability (2.70% median error in inter-beat interval) measurements. Unlike PPG, which exhibits variable performance across skin tones, our study shows that APG is resilient to variation in: skin tone, sub-optimal seal conditions, and ear canal size. More detailed evaluations can be found in the paper.
APG transforms any TWS ANC headphones into smart sensing headphones with a simple software upgrade, and works robustly across various user activities. The sensing carrier signal is completely inaudible and not impacted by music playing. More importantly, APG represents new knowledge in biomedical and mobile research and unlocks new possibilities for low-cost health sensing.
Acknowledgements
APG is the result of collaboration across Google Health, product, UX and legal teams. We would like to thank David Pearl, Jesper Ramsgaard, Cody Wortham, Octavio Ponce, Patrick Amihood, Sam Sheng, Michael Pate, Leonardo Kusumo, Simon Tong, Tim Gladwin, Russ Mirov, Kason Walker, Govind Kannan, Jayvon Timmons, Dennis Rauschmayer, Chiong Lai, Shwetak Patel, Jake Garrison, Anran Wang, Shiva Rajagopal, Shelten Yuen, Seobin Jung, Yun Liu, John Hernandez, Issac Galatzer-Levy, Isaiah Fischer-Brown, Jamie Rogers, Pramod Rudrapatna, Andrew Barakat, Jason Guss, Ethan Grabau, Pol Peiffer, Bill Park, Helen O'Connor, Mia Cheng, Keiichiro Yumiba, Felix Bors, Priyanka Jantre, Luzhou Xu, Jian Wang, Jaime Lien, Gerry Pallipuram, Nicholas Gillian, Michal Matuszak, Jakub Wojciechowski, Bryan Allen, Jane Hilario, and Phil Carmack for their invaluable insights and support. Thanks to external collaborators Longfei Shangguan and Rich Howard, Rutgers University and University of Pittsburgh.

